Artificial intelligence has been revolutionary throughout 2020 and has played a huge role in the development of the Covid vaccine. However, to understand how AI has been harnessed in the era of COVID-19, we first must analyze prior implementations as well as the science behind a vaccine.
How does a traditional vaccine work?
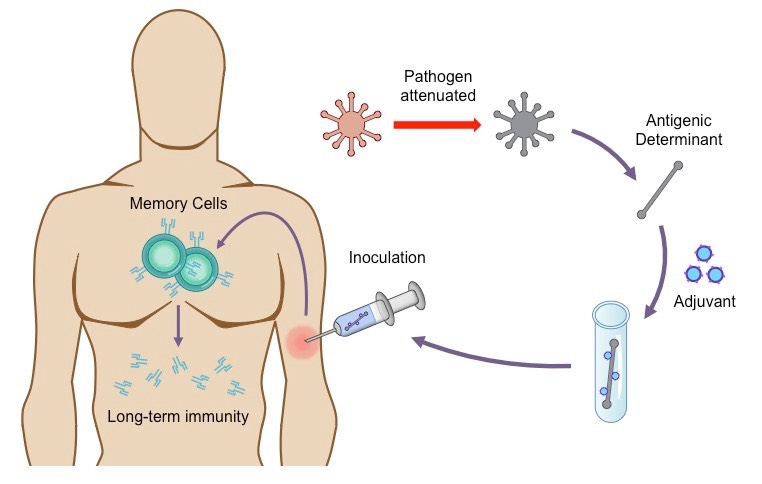
The goal of a vaccine is to prepare the body for an infection by pre-exposing the immune system to a weakened version of the virus. This early exposure enables to body to build up the tools to fight the virus at a later stage. But, how does this work? The key lies in the structure of the viruses themselves and how the immune system takes advantage of a virus’ weaknesses.
When the body is infected and has not already been vaccinated, the innate immune system toils to limit the spread of the virus as much as possible before the adaptive immune system can pick up the slack. T-cells circulate through the body, searching for human cells that have become infected, and they trigger processes to eliminate these infected cells by using Killer T-cells. This elimination prevents the virus from replicating.
Eventually, the adaptive immune system joins in, with B-cells recognizing antigens on the surface of the invader and connecting to the antigens of the virus. Binding to the antigens in this way interferes with the ability of the virus to infect new cells. Then Helper T-cells facilitate the mass-production of these B-cells, creating a factory for the virus-trapping antibodies that allow the body to stave away the infection [11]. At this point, the war is almost over, and the magic of the immune system comes into play once more in the embodiment of memory cells. These are re-purposed T and B-cells that retain the information about how to fight off the virus, and they remain with the body for a long time. If the same virus attempts an attack, the body can respond much more quickly and effectively, because these cells remember how to vanquish the virus that they had once fought [10].
The central theory behind the functionality of a vaccine exploits this knowledge; a successful vaccination introduces an antigen into the immune system by using a weakened source, such as a dead virus, thus allowing the creation of memory cells for future infections. In vaccine development, the arduous process is discovering which antigens will trigger immune responses that are safe and that minimize adverse side effects.
What roles can AI play in vaccine development?
AI or specifically machine learning is excellent for repetitive tasks that require big data analysis, making it apt for use in drug development. However, as biomedical data and computational power have expanded rapidly in the Age of the Internet, how to mine the large-scale chemistry data becomes a crucial problem for drug discovery. But, it is a problem that can be tackled with deep learning.
Notably, deep learning has been a useful tool in predicting the properties and activities of drug chemicals that could elicit a reaction with a virus in the body [4]. Automating this discovery process is incredibly powerful because this could typically take years of experimentation, pouring over literature and millions of dollars to explore [9].
Insight into viral structure is critical in the development of a vaccine. To best curate the specific proteins that will go into an immunization, scientists must understand where the virus can be attacked - regions on the virus called immunogenic sites. Researchers have been able to train models to predict what immunogenic sites to include in a vaccine such that the immune system can learn and be better prepared for the confrontation of those antigens specifically [7]. Associating this with specific proteins can then fast-track the vaccine development process, foregoing much of the typical trial and error. AI can also be useful in identifying antigens that have been identified in other pathogens that may be similar to antigens of the new virus, further hastening the process.
Another productive implementation of AI directly follows this pipeline. Once scientists have confirmed the structure of a virus, they can move forward with applying AI to predict which drugs could counteract the disease. When trained on existing compounds from databases such as Tox21 (a US federal toxicology database), these models can provide insight into which existing compounds would be effective; in the absence of such compounds, models can amazingly go even further and create new ones [1].
How has AI been used this year?
Now, how has AI revolutionized the drug development process this past year? In the paper entitled: “AI Can Help Scientists Find a Covid-19 Vaccine,” authors Etzioni and Decario cut straight to the chase, writing that AI is playing the crucial role of “suggesting components of a vaccine by understanding viral protein structures, and helping medical researchers scour tens of thousands of relevant researchers at an unprecedented pace” [6]. By contributing to the understanding of viral structure, AI greatly speeds up the development process because it gives scientists much insight into which compounds may be better suited to counteract the novel virus to function as therapeutics. Furthermore, such discernments about the structure of a virus can be instrumental in the development of an effective vaccine.
In tackling Covid-19, researchers at MIT’s Computer Science and Artificial Intelligence Laboratory (CSAIL) sharpened their focus on the spike proteins of the virus, a specific structure which can be targeted. CSAIL’s OptiVax machine learning algorithm introduces methods for designing new peptide vaccines, evaluating existing vaccines, and augmenting existing vaccine designs [2].
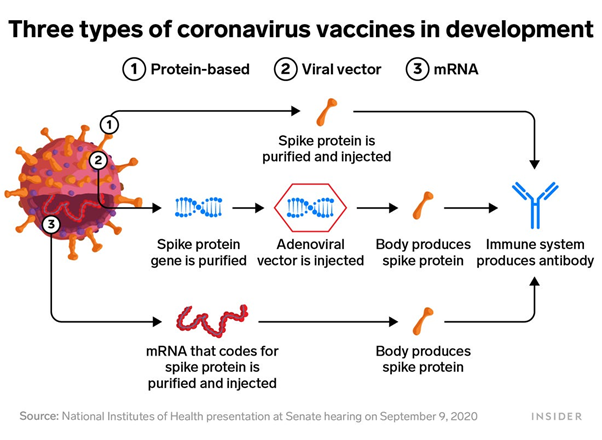
Spike proteins are incredibly important in current COVID-19 vaccine development because they include antigens that can be recognized and attacked by the immune system, something that machine learning was able to deduce very early on in the pandemic, which later research confirmed that recovered patients’ antibodies were binding to [7]. OptiVax can consequently design a collection of peptides such that they create the most immuno-coverage in the population.
Another example of how advantageous AI methods can be when battling a virus comes from a Stanford University by Ethan Fast, Russ B. Altman, and Binbin Chen published in March of 2020 in BioRxiv. These researchers had the foresight in February to computationally predict the structure of the novel coronavirus with the intent of identifying “T-cell and B-cell epitopes [an antigen targeted by T-cells and B-cells] based on viral protein antigen presentation and antibody binding properties” [8]. At such an early stage in the pandemic, AI amazingly provided the researchers with the insight that spike proteins on coronavirus were viable epitopes to include in a vaccine candidate or target with drugs because of the stability of the genome around the spike protein, unlike much of the viral genome which changes rapidly. Keep in mind, this work was done in February, light-years ahead of the traditional vaccine or antiviral development pipeline at the time; clearly, AI is a tool of extreme acceleration beyond the accepted methods of response to diseases.
Social implications
Yet, the scope of AI in addressing this calamity has also reached a social sphere of influence. Researchers at MIT’s CSAIL recently trained a machine learning model to analyze the performance of vaccines similar to the leading candidates of Moderna and Pfizer. After analyzing the performance of the vaccine on different patient populations, the research team found that “among white participants, the amount of people whose immune systems didn’t strongly respond to the vaccine was less than half of one percent,” while “among Asian participants, that figure was nearly ten percent”[12]. Such disparities are unfortunately built into the drug development system, and AI is doing its part in bringing this to light. Clinical trials have historically undersampled members of underrepresented communities in science and leadership, leading to differing, often subpar results for certain subpopulations when it comes to applying drugs to broader groups of people. Thus, this discovery by CSAIL is crucial in ensuring equity as the world heals.
But, AI’s role in addressing the pandemic in society doesn’t stop there: CSAIL also constructed a machine learning model “for improving the vaccines’ effectiveness in certain populations” [12]. This “augmentation” strategy functions to include additional peptides in the COVID-19 vaccine for certain populations, which has been key in ensuring that the vaccine is almost completely effective across every ethnic boundary. CSAIL’s discoveries are critical as we navigate a world with inequality at every turn, ensuring fairness in the vaccine development process that has previously been neglected by much of science.
To wrap up
AI is by no means a perfect solution to the COVID-19 crisis. A massive underlying problem in the intersectionality of machine learning and medicine is access to data; many patients, reasonably so, have concerns over the trustworthiness of AI models. Furthermore, issues of data privacy and security come to bear when using AI in healthcare environments. Additionally, our models are only as good as the datasets that we feed them, thus every model’s prediction must be taken with a grain of salt when weighing in the variance and prejudices from the data it has. It is also accepted that AI is prone to bias, overfitting, and discrimination.
The whole purpose of implementing machine learning is to greatly speed up and cheapen the developmental process, but there are certain measures that must always be taken before a product is released to the public to ensure that models promote equity over perpetuating disparity [3]. Hopefully, as this method improves, we can significantly reduce the time that we wait for vaccines and antivirals, as well as make the process much cheaper without sacrificing the health of patients. However, while AI can boost the scientific method, it cannot not replace it.
References
- Abd-Alrazaq Mohannad Alajlani; , Alaa. “Artificial Intelligence in the Fight against COVID-19: A Scoping Review.” JMIR Preprints, 27 May 2020, preprints.jmir.org/preprint/20756/accepted.
- By, Written, and Rachel Gordon. “Potential COVID-19 Vaccines Get a Boost from Machine Learning.” Potential COVID-19 Vaccines Get a Boost from Machine Learning | MIT CSAIL, 27 July 2020, www.csail.mit.edu/news/potential-covid-19-vaccines-get-boost-machine-learning.
- Chandra Kaushik, Aman, and Utkarsh Raj. “AI-Driven Drug Discovery: A Boon against COVID-19?” AI Open, The Authors. Published by Elsevier B.V. on Behalf of KeAi Communications Co., Ltd., 2020, www.ncbi.nlm.nih.gov/pmc/articles/PMC7396325/.
- Chen, Hongming, et al. “The Rise of Deep Learning in Drug Discovery.” Drug Discovery Today, Elsevier Current Trends, 31 Jan. 2018, www.sciencedirect.com/science/article/pii/S1359644617303598?via=ihub.
- “Department of Health.” The Science Behind Vaccine Research and Testing, 2014, www.health.ny.gov/prevention/immunization/vaccine_safety/science.htm.
- Etzioni, Oren. “AI Can Help Scientists Find a Covid-19 Vaccine.” Wired, Conde Nast, Mar. 2020, www.wired.com/story/opinion-ai-can-help-find-scientists-find-a-covid-19-vaccine/.
- Fast, Ethan, and Binbin Chen. “Can Artificial Intelligence Help Us Design Vaccines?” Brookings, Brookings, 30 Apr. 2020, www.brookings.edu/techstream/can-artificial-intelligence-help-us-design-vaccines/.
- Fast, Ethan, et al. “Potential T-Cell and B-Cell Epitopes of 2019-NCoV.” BioRxiv, Cold Spring Harbor Laboratory, 1 Jan. 2020, www.biorxiv.org/content/10.1101/2020.02.19.955484v2.
- Hughes, J P, et al. “Principles of Early Drug Discovery.” British Journal of Pharmacology, Blackwell Science Inc, Mar. 2011, www.ncbi.nlm.nih.gov/pmc/articles/PMC3058157/.
- Kazilek. Memory B-Cell, 4 Aug. 2011, askabiologist.asu.edu/memory-b-cell.
- Kazilek. “T-Cells.” Kazilek, 16 Feb. 2011, askabiologist.asu.edu/t-cell.
- Kent, Jessica. “AI Shows COVID-19 Vaccines May Be Less Effective in Racial Minorities.” HealthITAnalytics, 3 Dec. 2020, healthitanalytics.com/news/ai-shows-covid-19-vaccines-may-be-less-effective-in-racial-minorities.
- Publishing, Harvard Health. “What You Should Know about Antiviral Drugs.” Harvard Health, Dec. 2015, www.health.harvard.edu/drugs-and-medications/what-you-should-know-about-antiviral-drugs.
- Secretary, HHS Office of the, and Assistant Secretary for Public Affairs (ASPA). “Fact Sheet: Explaining Operation Warp Speed.” HHS.gov, US Department of Health and Human Services, 30 Nov. 2020, www.hhs.gov/coronavirus/explaining-operation-warp-speed/index.html.
- Vaishya, Raju, et al. “Artificial Intelligence (AI) Applications for COVID-19 Pandemic.” Diabetes & Metabolic Syndrome: Clinical Research & Reviews, Elsevier, 14 Apr. 2020, www.sciencedirect.com/science/article/pii/S1871402120300771.
- Vamathevan, Jessica, et al. “Applications of Machine Learning in Drug Discovery and Development.” Nature Reviews. Drug Discovery, U.S. National Library of Medicine, June 2019, www.ncbi.nlm.nih.gov/pmc/articles/PMC6552674/.

